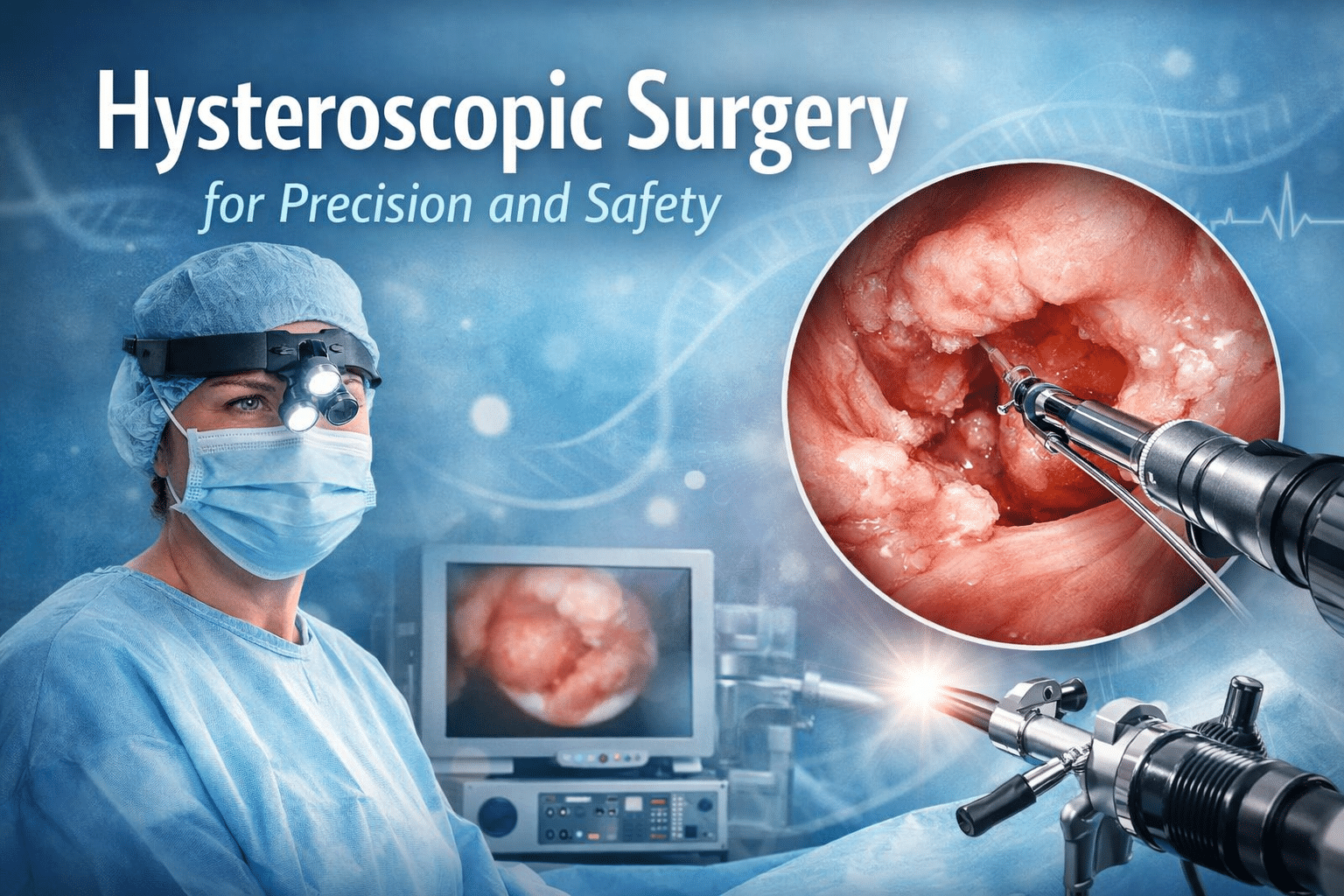
Hysteroscopic surgery represents one of the most significant advancements in minimally invasive gynecological procedures.
By allowing direct visualization and treatment of intrauterine pathology without external incisions, hysteroscopic techniques have transformed both diagnostic and operative gynecology.
Modern hysteroscopic surgery combines optical clarity, controlled energy delivery, and refined instrumentation to address a wide range of uterine conditions with high precision and reduced patient morbidity.
As healthcare systems increasingly emphasize patient safety, faster recovery, and procedural efficiency, hysteroscopic surgery has become a standard approach in many gynecological practices.
The integration of electrosurgical technologies, particularly bipolar energy systems compatible with saline irrigation, has further enhanced the safety profile and clinical effectiveness of these procedures.
This article explores hysteroscopic surgery from a technical and clinical perspective, highlighting its principles, applications, and growing importance in modern gynecology.
Explore Lamidey-Noury solutions for minimally invasive surgery!
Article Index
-
What Is Hysteroscopic Surgery?
-
How Hysteroscopic Surgery Is Performed?
-
Diagnostic vs Operative Hysteroscopy
-
Role of Electrosurgery in Hysteroscopic Surgery
-
Bipolar Technology in Hysteroscopic Procedures
-
Importance of Irrigation and Fluid Management
-
Safety and Precision in Hysteroscopic Surgery
-
Clinical Benefits for Gynecologists
-
Benefits for Hospitals and Day Surgery Units
-
Future Trends in Hysteroscopic Surgery Technology
1. What Is Hysteroscopic Surgery?
Hysteroscopic surgery is a minimally invasive gynecological procedure that allows direct examination and treatment of the uterine cavity using a hysteroscope.
The hysteroscope is a thin, rigid or flexible instrument equipped with an optical system and working channels that enable the introduction of surgical instruments. It is inserted through the vagina and cervix, eliminating the need for abdominal incisions.
The primary purpose of hysteroscopic surgery is to diagnose and treat intrauterine abnormalities such as polyps, submucosal fibroids, adhesions, congenital uterine anomalies, and causes of abnormal uterine bleeding.
By providing direct visualization, hysteroscopy allows targeted intervention with a high degree of accuracy.
From a technical standpoint, hysteroscopic surgery relies on controlled distension of the uterine cavity using fluid media, precise optical imaging, and carefully regulated energy sources when operative intervention is required.
This combination enables surgeons to perform delicate procedures while preserving surrounding tissue.
In modern gynecology, hysteroscopic surgery is valued not only for its clinical effectiveness but also for its patient-centered advantages.
Reduced postoperative pain, shorter recovery times, and lower complication rates make it an attractive alternative to traditional open or laparoscopic approaches for selected indications.
2. How Hysteroscopic Surgery Is Performed?
The performance of hysteroscopic surgery involves a carefully coordinated sequence of steps designed to ensure safety, visibility, and procedural efficiency.
After appropriate patient preparation and cervical access, the hysteroscope is gently introduced into the uterine cavity. Continuous visualization allows the surgeon to assess the anatomy and identify pathological findings.
Uterine distension is achieved using an irrigation fluid, which expands the cavity and improves visualization. The choice of fluid depends on the type of procedure and the energy system used.
Modern hysteroscopic surgery increasingly favors saline irrigation, particularly when bipolar electrosurgical systems are employed.
Once the pathology is identified, operative instruments such as scissors, graspers, or electrosurgical electrodes are introduced through the working channels of the hysteroscope.
Energy delivery, when required, is precisely controlled via an electrosurgery generator, allowing targeted tissue resection or coagulation.
Throughout the procedure, continuous monitoring of fluid balance, energy output, and visualization is essential. This controlled environment enables surgeons to perform complex intrauterine interventions with minimal trauma and predictable outcomes.
Discover advanced electrosurgical platforms!
3. Diagnostic vs Operative Hysteroscopy
Hysteroscopic surgery encompasses both diagnostic and operative procedures, each serving distinct clinical purposes. Diagnostic hysteroscopy focuses on visual assessment of the uterine cavity to identify abnormalities that may not be detected through imaging alone.
It is commonly used in the evaluation of abnormal uterine bleeding, infertility, and recurrent pregnancy loss.
Operative hysteroscopy, on the other hand, involves active surgical intervention to treat identified pathology. Procedures such as polypectomy, myomectomy, adhesiolysis, and septum resection are performed under direct visualization, often using electrosurgical energy.
The transition from diagnostic to operative hysteroscopy can often occur within the same session, improving efficiency and patient convenience. This “see and treat” approach reduces the need for multiple procedures and hospital visits.
From a technical perspective, operative hysteroscopy demands higher levels of precision, reliable energy control, and effective fluid management. Advances in instrumentation and energy systems have significantly expanded the scope and safety of operative hysteroscopic surgery.
Stay updated with the latest innovations and clinical insights!
4. Role of Electrosurgery in Hysteroscopic Surgery
Electrosurgery plays a central role in operative hysteroscopic procedures by enabling controlled tissue cutting and coagulation. High-frequency electrical energy is delivered through specialized electrodes designed for intrauterine use, allowing precise interaction with targeted tissue.
The electrosurgery generator regulates energy output, adapting to tissue characteristics and procedural requirements. This control is essential for minimizing thermal spread and preserving healthy endometrial tissue.
In hysteroscopic surgery, electrosurgery is commonly used for resection of fibroids, removal of polyps, and coagulation of bleeding vessels. The ability to combine cutting and coagulation functions improves efficiency and reduces operative time.
Modern electrosurgical systems designed for hysteroscopy emphasize safety, stability, and compatibility with saline irrigation. These features align with current clinical standards and support consistent surgical performance.
Learn more about electrosurgery generator technology!
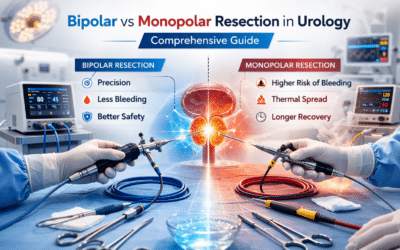
5. Bipolar Technology in Hysteroscopic Procedures
Bipolar technology has become increasingly important in hysteroscopic surgery due to its localized energy delivery and enhanced safety profile. In bipolar systems, electrical current flows between two closely spaced electrodes at the surgical site, limiting energy dispersion.
This confined energy pathway allows the use of saline irrigation, which is physiologically compatible and reduces the risk of fluid-related complications. Bipolar technology also provides improved hemostasis and consistent tissue interaction.
In hysteroscopic procedures, bipolar instruments support precise resection and coagulation while maintaining a clear surgical field. Their reliability makes them particularly suitable for complex or prolonged procedures.
The adoption of bipolar technology reflects a broader trend toward safer, more controlled energy-based surgery in gynecology.
Explore bipolar electrosurgical technologies!
6. Importance of Irrigation and Fluid Management
Effective irrigation and fluid management are essential components of hysteroscopic surgery. Irrigation fluid serves to distend the uterine cavity, improve visualization, and remove blood and debris from the surgical field.
Saline irrigation is increasingly preferred, particularly when bipolar energy systems are used. Its physiological compatibility reduces the risk of electrolyte imbalance and systemic absorption complications.
Careful monitoring of fluid inflow and outflow is critical to patient safety. Advances in hysteroscopic equipment have improved fluid control, supporting safer and more predictable procedures.
Optimized irrigation contributes directly to surgical precision, visibility, and overall procedural success.
Learn about Lamidey-Noury quality and safety standards
7. Safety and Precision in Hysteroscopic Surgery
Safety and precision are defining characteristics of hysteroscopic surgery. Direct visualization allows surgeons to target pathology accurately while preserving healthy tissue.
Controlled energy delivery and saline irrigation further enhance safety by minimizing thermal and systemic risks. These factors contribute to lower complication rates and improved patient outcomes.
Modern hysteroscopic systems are designed to support consistent performance and compliance with international safety standards, reinforcing their role in contemporary gynecological practice.
8. Clinical Benefits for Gynecologists
For gynecologists, hysteroscopic surgery offers enhanced diagnostic accuracy, precise treatment options, and efficient workflow. Reduced operative time and predictable outcomes support professional confidence and procedural consistency.
The minimally invasive nature of hysteroscopy also aligns with patient expectations for faster recovery and lower morbidity.
9. Benefits for Hospitals and Day Surgery Units
From an institutional perspective, hysteroscopic surgery supports efficient use of operating rooms and resources. Shorter procedures, reduced hospital stays, and lower complication rates contribute to cost optimization.
Standardized hysteroscopic platforms also simplify training and equipment management, supporting sustainable healthcare delivery.
10. Future Trends in Hysteroscopic Surgery Technology
The future of hysteroscopic surgery is driven by innovation in optics, energy delivery, and digital integration. Advances in bipolar technology, smart energy modulation, and ergonomic instrument design continue to expand the capabilities of hysteroscopic procedures.
These developments reinforce hysteroscopic surgery as a cornerstone of modern minimally invasive gynecology.